“`html
Essential Guide to Understanding Frostbite
What is Frostbite and Its Causes?
**Frostbite** is a serious condition caused by freezing of body tissues, often affecting extremities such as fingers, toes, ears, and the nose. This injury typically occurs in frigid conditions, particularly when skin is exposed to outdoor elements. The increasing wind chill significantly escalates the risk of frostbite, with the likelihood rising dramatically when temperatures drop below 30°F (-1°C). Understanding the **causes of frostbite** is crucial for prevention. Prolonged exposure to cold, especially combined with moisture, can compromise blood flow and lead to this condition. Individuals with certain health conditions like diabetes or those at high altitudes face further risks.
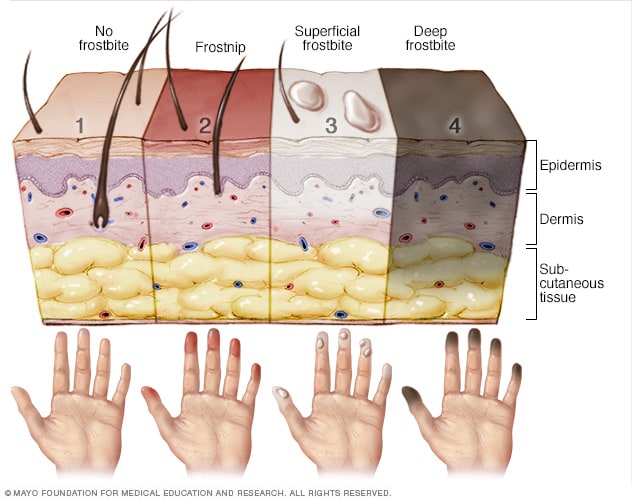
Understanding the Stages of Frostbite
Frostbite develops in stages, impacting the severity of tissue injury. The first stage, known as frostnip, is a mild form where the skin appears red and feels cold without permanent damage. As frostbite progresses, symptoms evolve through varying **frostbite severity levels**: superficial frostbite often causes the affected skin to morph into a pale color and may involve blistering, while deep frostbite presents a more severe threat, potentially leading to tissue death. Recognizing these stages is vital; immediate intervention can prevent complications.
Factors Influencing the Development of Frostbite
Several environmental and individual factors influence how quickly frostbite occurs. Key determinants include exposure time, temperature, humidity, and wind speed. For instance, **outdoor exposure conditions** radically determine susceptibility to frostbite. It’s important to note that certain groups, like children and the elderly, are at heightened risk due to their skin’s sensitivity and lower overall body heat. This reinforces why understanding the risks, such as in **frostbite in children**, is critical for ensuring safety during winter activities.
Recognizing Symptoms and Signs of Frostbite
**Symptoms of frostbite** are crucial for early diagnosis and treatment. The first signs often include unusual tingling sensations or itching, followed by numbness as the condition worsens. As it progresses, affected areas, particularly **frostbite on fingers** or **frostbite on toes**, may appear red initially, followed by paleness, hardening, and eventually the development of blisters. For those exposed to extreme cold, recognizing these **mild frostbite signs** can make a difference in saving potentially damaged tissue.
Severe Symptoms: When to Seek Medical Attention
Severe frostbite can result in significant tissue damage, necessitating **frostbite medical attention**. Symptoms of more advanced frostbite include darkened skin, severe pain, or gangrene, indicating tissue death. If these symptoms appear, it is essential to act promptly and seek immediate medical care. Understandably, knowing when to recognize these signs can mitigate severe consequences, including potential amputations, hence the importance of addressing the **symptoms of severe frostbite**.
Documenting Symptoms Timeline for Frostbite
Upon experiencing symptoms of frostbite, a clear timeline can aid in both personal and medical discussions. The **symptoms timeline for frostbite** often unfolds rapidly within 30 minutes of exposure in severe cold conditions. This timeline will help to guide responses in medical emergencies, increasing awareness and efficacy in treatment protocols. Moreover, documenting such experiences provides valuable insights into **frostbite awareness**, enhancing preventative education.
Treatment Options for Frostbite
Understanding the appropriate **treatment for frostbite** is vital for recovery. For initial stages, gradually warming the affected areas with body heat or warm water may help restore blood flow without causing further damage. Over-the-counter pain relievers can alleviate discomfort, while severe frostbite may require medical interventions such as intravenous fluids or even surgery. Establishing a comprehensive **frostbite treatment protocol** enhances recovery outcomes and ensures effective management.
First Aid Steps for Mild Frostbite
Administering proper **frostbite first aid** can significantly impact mild cases of frostbite. Gently warming the affected areas is the core principle. Avoid rubbing the frostbitten area since this can exacerbate the injury. Instead, use warm (not hot) water to immerse the area or apply warm, dry cloths for gradual rewarming. Furthermore, drying and covering the area post-warming can inhibit further exposure, safeguarding against **frostbite effects on skin**.
Caring for Moderate to Severe Frostbite
In cases of **severe frostbite**, professional medical care is often required. Medical teams will assess the severity and the potential for skin grafts if cell death is apparent. Post-treatment follow-ups are critical in monitoring the recovery process to avoid secondary complications. Moreover, proper **frostbite recovery** protocols, including rehabilitation techniques that enhance blood flow and minimize tissue damage, are essential in restoring functionality.
Preventing Frostbite: Tips and Strategies
Prevention remains the best approach to avoid frostbite. Different strategies can help mitigate risks such as dressing warmly in layers and minimizing skin exposure during outdoor activities. Awareness of **frostbite prevention tips** such as choosing appropriate clothing, checking the weather forecasts, and preparing for **frostbite risks** due to altitude or wind are all essential steps. Knowledge surrounding these factors equips individuals to fully prepare and safeguard themselves.
Understanding the Hypothermia Relationship with Frostbite
There is a critical connection between **hypothermia** and frostbite, both stemming from cold exposure. When body temperature drops, blood flow to extremities decreases, increasing the likelihood of frostbite. Recognizing this relationship allows individuals to take necessary precautions when exposed to frigid environments. Safety steps against low temperatures should always consider the interconnected risks of these conditions.
Behavioral Changes for Frostbite Prevention
To combat frostbite effectively, embracing behavioral changes is crucial. Planning breaks indoors when engaged outdoors helps to manage exposure times, while staying hydrated enhances circulation. Lastly, educating oneself and others, especially children, on how to **avoid frostbite** will foster responsible attitudes and effective action when engaging in winter sports or activities.
Key Takeaways
- Frostbite can be prevented through appropriate clothing and situational awareness.
- Symptoms evolve through various stages; early detection drastically improves outcomes.
- Treatment varies significantly from mild to severe, emphasizing the need for prompt care.
- Understanding environmental factors plays a key role in the prevention and management of frostbite.
- Behavioral modifications and education help build awareness and strategies to avoid frostbite.
FAQ
1. How quickly does frostbite develop under extreme conditions?
Frostbite can develop in as little as 30 minutes under extremely cold conditions. Wind chill may lead to faster onset, making prompt action necessary to avoid tissue damage.
2. What are the critical temperatures for frostbite risk?
Frostbite can begin at temperatures below 32°F (0°C). However, risks escalate dramatically under zero degrees Fahrenheit, particularly when coupled with moist skin or high wind conditions.
3. What constitutes as frostbite first aid?
Frostbite first aid includes rewarming the affected area with warm water immersion or body heat. Avoid rubbing the area as it could cause further tissue injury and damage.
4. What are the signs differentiating frostbite from chilblains?
Chilblains present as painful, itchy swellings on the skin after being exposed to cold. In contrast, frostbite can cause blistering and significant skin discoloration indicating deeper tissue damage.
5. When should I seek medical help for frostbite?
Seek medical help if severe symptoms arise, such as intense pain, changes in skin color to dark hues, or if symptoms worsen despite at-home treatment.
“`